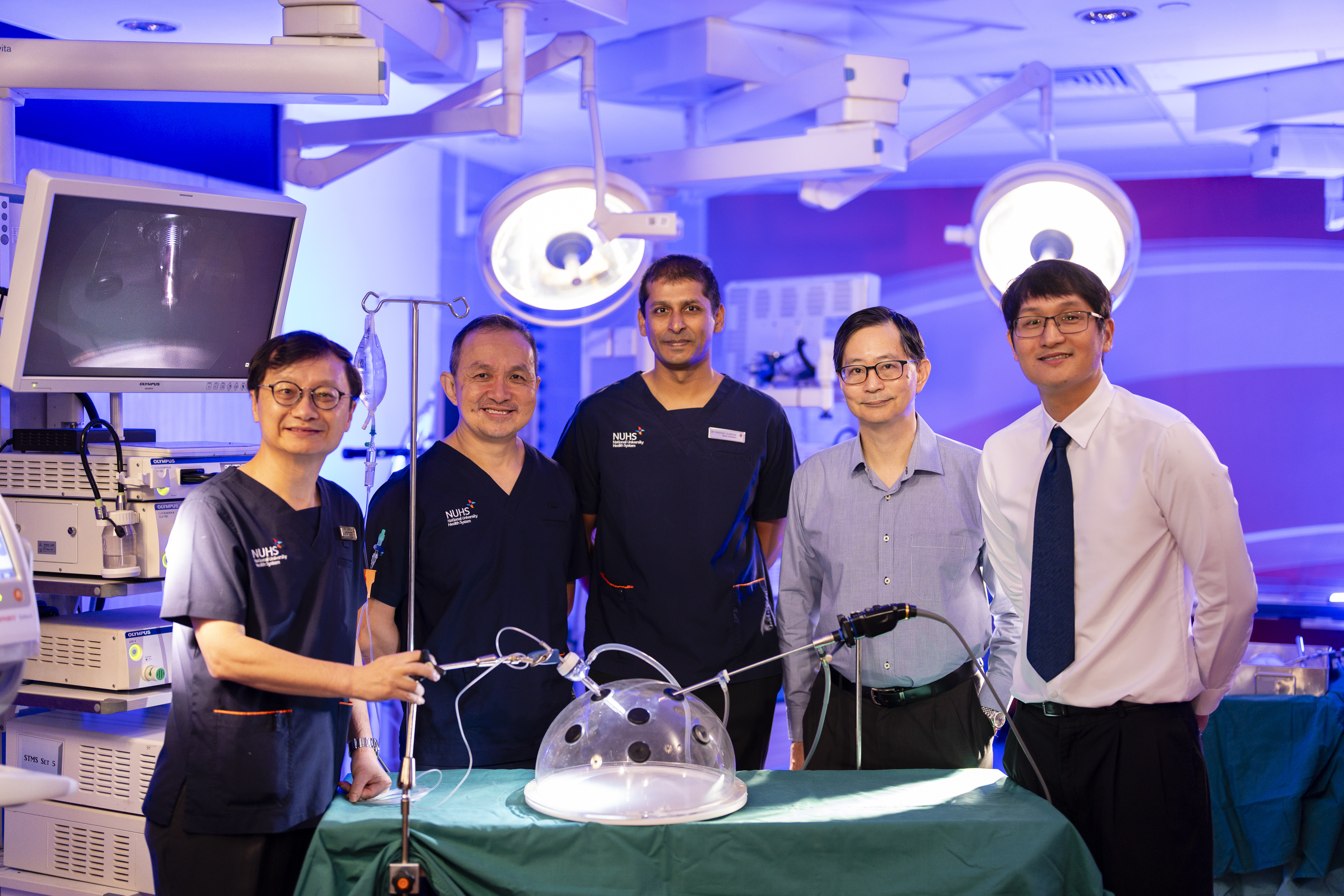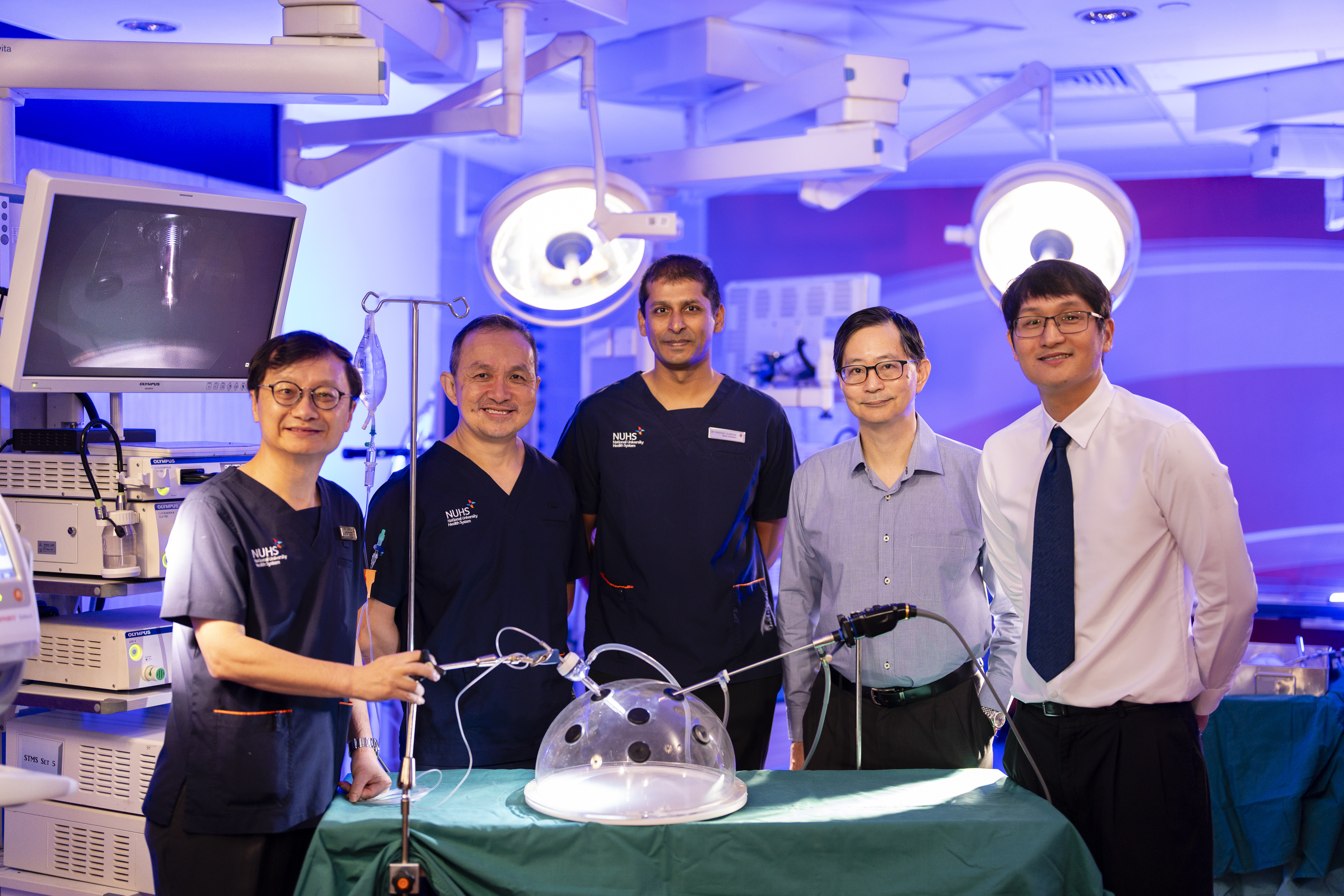
From left: Prof Jimmy So, Senior Consultant, Head of the Division of General Surgery (Upper Gastrointestinal Surgery), NUH; Dr Yong Wei Peng, Senior Consultant, Department of Haemotology-Oncology, NCIS; Dr Raghav Sundar, Senior Consultant, Department of Haemotology-Oncology, NCIS; Prof Patrick Tan, Senior Vice-Dean for Research, Duke-NUS Medical School; A/Prof Johnny Ong, Senior Consultant, Department of Sarcoma, Peritoneal and Rare Tumours, Division of Surgery and Surgical Oncology, SGH and NCCS. (Photo credit: NUH)
Singapore — Gastric cancer remains a formidable adversary, ranking as the fifth most common cancer and the third-leading cause of cancer-related deaths worldwide, with over 1,000,000 new cases and close to 770,000 deaths each year. In Singapore, gastric cancer ranks among the top 10 causes of cancer-related deaths and claims about 300 lives each year.
The peritoneum, the lining of the abdominal cavity, is frequently involved in advanced stage cancers, including gastric, colon, pancreatic, and ovarian cancers. For gastric cancer, the peritoneum is, in fact, the most common site of metastasis, both before and after treatments. Patients with gastric cancer peritoneal metastases (GCPM) often face an exceptionally grim prognosis, with severe symptoms and rapid disease progression. Median survival rates range from just three to six months, and five-year survival rates are usually below five per cent. Therapeutic options are currently limited.
In a major breakthrough, clinicians and scientists from Singapore have shed light on the intricate mechanisms behind the spread of gastric cancer to the peritoneum. This landmark research, published in the prestigious journal Gastroenterology, offers renewed hope for patients battling this aggressive form of cancer. The scientists also conducted a clinical trial, published in another journal ESMO Open, demonstrating the safety and potential of a novel treatment approach for the disease.
The research study, spearheaded by a team of clinicians and scientists from the National University Hospital (NUH), the National University Cancer Institute, Singapore (NCIS), the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine), the National Cancer Centre Singapore (NCCS) and Duke-NUS Medical School, utilised cutting-edge genomic and transcriptomic technologies to analyse a vast collection of patient samples.
This in-depth analysis has provided an unparalleled understanding of the molecular underpinnings of gastric cancer peritoneal spread.
Dr Raghav Sundar, Senior Consultant in the Department of Haematology-Oncology at NCIS, who led the study published in Gastroenterology, emphasised: “Our research has pulled back the curtain on the complex biological processes that drive the spread of gastric cancer to the peritoneum. These findings provide a crucial roadmap for developing more effective and targeted treatments for this devastating disease.” Dr Sundar is also Associate Professor of Medicine at NUS Medicine.
Understanding the difficult terrain of peritoneal spread
The new findings not only shed light on why gastric cancer cells tend to metastasise to the peritoneum, but also pave the way for the development of innovative therapies that target the cells and molecules surrounding the tumour – also known as the tumour microenvironment (TME), potentially disrupting the cancer’s ability to thrive in the peritoneum.
Key findings from the research include: -
- Unravelling the peritoneal connection: The research pinpointed specific genetic alterations and characteristics within the TME that contribute to the spread, or metastasis, of gastric cancer to the peritoneum. The TME is the complex network of cells and molecules surrounding a tumour. This discovery explains why gastric cancer cells have a tendency to spread to the peritoneum.
- The tumour microenvironment's pivotal role: The study underscores the crucial role of the TME in facilitating the establishment and growth of peritoneal metastases. This newfound understanding paves the way for the development of innovative therapies that target the TME, potentially disrupting the cancer's ability to thrive in the peritoneum.
- Identifying biomarkers and therapeutic targets: The researchers successfully identified potential biomarkers that could predict the risk of peritoneal metastasis, enabling earlier detection and intervention. Furthermore, they uncovered novel therapeutic targets that could be leveraged to develop more effective treatments specifically for GCPM.
“Prior to our study, there was limited understanding of the tumour microenvironment that contributes to the spread of gastric cancer to the peritoneum. Yet, most cancer patients do not die from their primary tumour but from its metastases to other organs. Our results highlight the complexity of gastric cancer metastases, revealing that gastric tumours can use distinct genetic and molecular mechanisms to spread to different organs,” said Professor Patrick Tan, Senior Vice-Dean for Research at Duke-NUS and one of the senior authors of the study.
Promising clinical trial
In a parallel development, the same research team conducted a clinical trial that showcased the safety and potential efficacy of a groundbreaking treatment approach for GCPM. The Phase I PIANO trial, published in ESMO Open, combined a minimally invasive surgical technique called Pressurised Intra-Peritoneal Aerosol Chemotherapy (PIPAC) with systemic immunotherapy. PIPAC delivers chemotherapy directly to the peritoneal cavity as a fine mist, while immunotherapy helps the body's immune system recognise and attack cancer cells.
This innovative approach aims to bolster the immune system's capacity to combat cancer within the peritoneal cavity. The trial results were promising, demonstrating that the combination therapy was well-tolerated by patients and resulted in a reduction in tumour burden for some. Importantly, molecular profiling of tumour samples revealed an increase in T-cell infiltration, a sign of a positive immune response against the cancer.
The trial was conducted from June 2020 to November 2022 with 18 patients recruited across three cancer centres—two centres in Singapore and one in Belgium.
“The PIANO trial results are incredibly encouraging, demonstrating the potential of combining targeted therapy like PIPAC with immunotherapy to improve outcomes for patients,” said Professor Jimmy So, Senior Consultant and Head of the Division of General Surgery (Upper Gastrointestinal Surgery) at NUH, who led the PIANO trial. “This approach could revolutionise the treatment landscape for this challenging condition.” Professor So is also Head & Senior Consultant, Division of Surgical Oncology, at NCIS, and Professor of Surgery at NUS Medicine.
Paving the way forward
The combined research endeavours mark a significant leap forward in the fight against GCPM. The identification of predictive biomarkers and therapeutic targets could lead to the development of personalised treatment strategies, tailoring treatments to the unique molecular profile of each patient's tumour. The success of the PIANO trial heralds a new era of combination therapies that leverage the power of the immune system to combat peritoneal metastases.
“Our research brought together leaders from multiple institutions who treat and diagnose gastric cancer and clinician-scientists who study the disease,” said Associate Professor Johnny Ong, Senior Consultant in the Department of Sarcoma, Peritoneal and Rare Tumours, Division of Surgery and Surgical Oncology, in Singapore General Hospital and NCCS who is co-author of the Gastroenterology study and co-investigator of the PIANO trial. “Combining bench and bedside research, we have shed new light on the biology of gastric cancer which will pave the way for the much-needed therapeutics in patients with peritoneal metastases.”
The studies are supported by the Singapore Gastric Cancer Consortium, a national translational research group comprising clinicians and scientists working in gastric cancer research from academic medical centres, universities, hospitals and research institutes across Singapore. It receives funding from the National Research Foundation Singapore under its Open Fund-Large Collaborative Grant, administered by the Singapore Ministry of Health’s National Medical Research Council.
To download the PDF version of the media release, click here.