A Practical Approach Towards Value Driven Outcomes in National University Polyclinics: Our Experience with VDO on Diabetes Mellitus
Case study
Background
Value-driven outcomes (VDO) seek to improve quality and outcomes for patients while rationalising the costs required to provide the desired quality care and outcomes for patients. Diabetes mellitus (DM) is one of the top three chronic conditions seen in the National University Polyclinics (NUP) and a risk factor for atherosclerotic cardiovascular disease. This chronic condition has multiple recommended care components that we have been monitoring quarterly in the past. With VDO, we are now aware of the associated bill size. In 2019, our polyclinics saw around 54,000 patients with DM and account for 148,000 follow-up visits that year.
Objectives
We share a practical approach to gather data and a simple dashboard for presentation to NUP Clinic Heads to understand clinical quality and bill size variability and to support value improvement initiatives. We designed a system that does not involve manual data entry so that clinic leadership and clinicians can focus on clinical care and value improvement.
Methodology
We engaged Family Physicians at NUP with interest in the management of diabetes mellitus to be Clinician Leads for VDO Diabetes Mellitus.
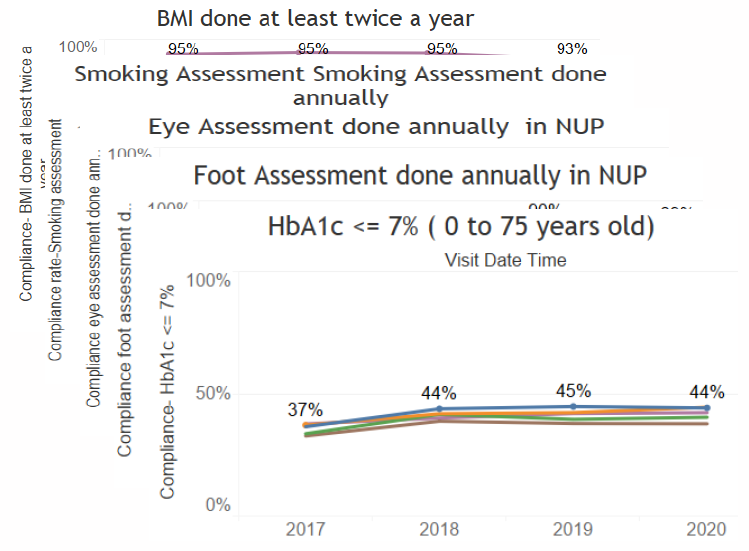
For the combined Clinical Quality Index (CQI), we identified HbA1c ≤ 7% (75 years old), HbA1c ≤ 8% (> 75 years old), HbA1c done (2 times annually), blood pressure measurement done (≥ 2 times annually), body mass index measurement done (≥ 1 time annually), lipid profile done (≥ 1 time annually), smoking assessment done (≥ 1 time annually), eye assessment done (≥ 1 time annually), foot assessment done (≥ 1 time annually) and nephropathy assessment done (≥ 1 time annually) as the components.
For bill size, we identified doctor consultations, care manager consultations, advanced practice nurse consultations, allied health professional consultations, metformin, glipizide, gliclazide, tolbutamide, sitagliptin, linagliptin, dapagliflozin, empagliflozin, acarbose, NPH insulin, glargine, levemir, regular insulin, aspart, glulisine, Mixtard-30, Novomix 30, HbA1c, diabetes monitoring panel, hypertension panel, lipid panel, diabetic retinal photography, diabetic foot screening, creatinine, protein-creatinine ratio, albumin-creatinine ratio, ECG and glucose that are related to care.
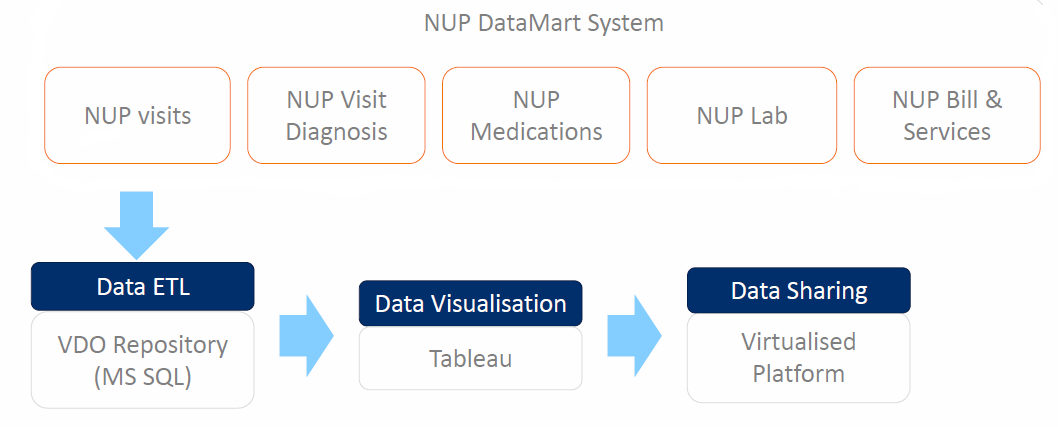
During each quarter, data from the clinical and administrative systems are extracted and loaded onto a NUP VDO database.
Data Sources
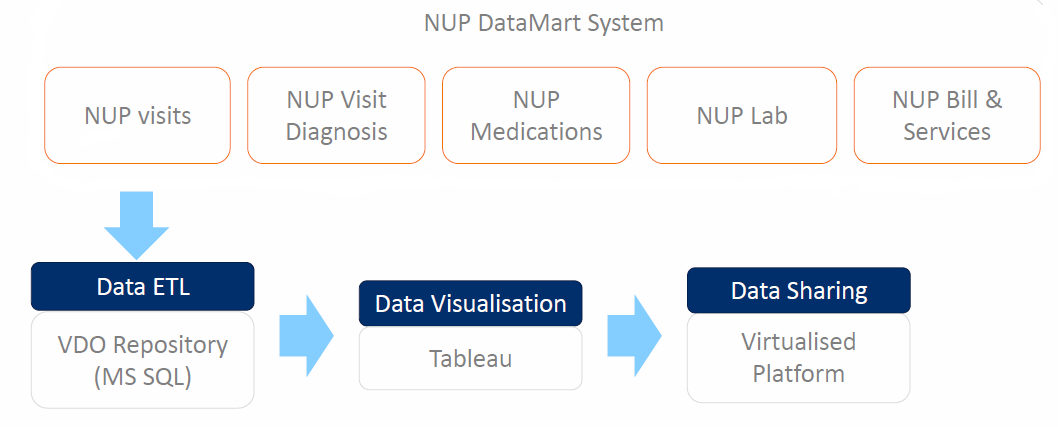
The charts are presented using Tableau to show the quarterly trends for CQI vs Bill Size, CQI breakdown, demographics, mean total bill breakdown, breakdown of drugs used, etc.
Results
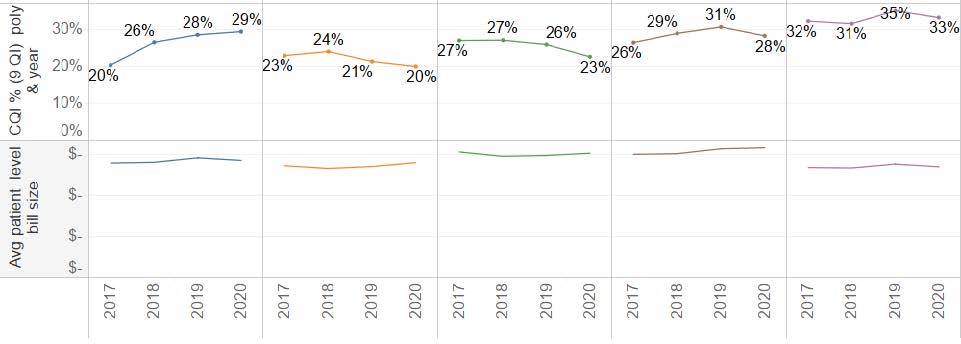
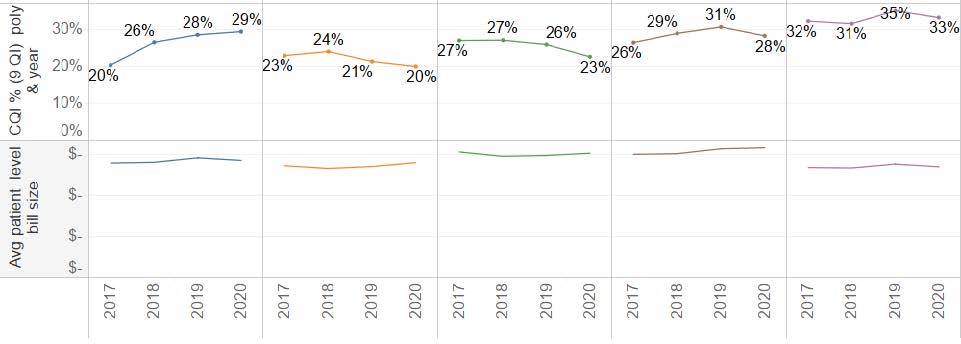
CQI vs Bill Size (2017 to 2020)
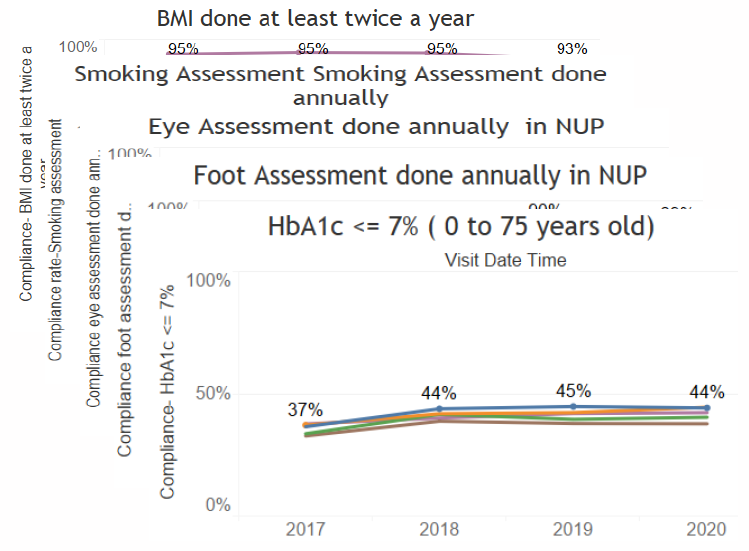
CQI Breakdown (2017 to 2020)
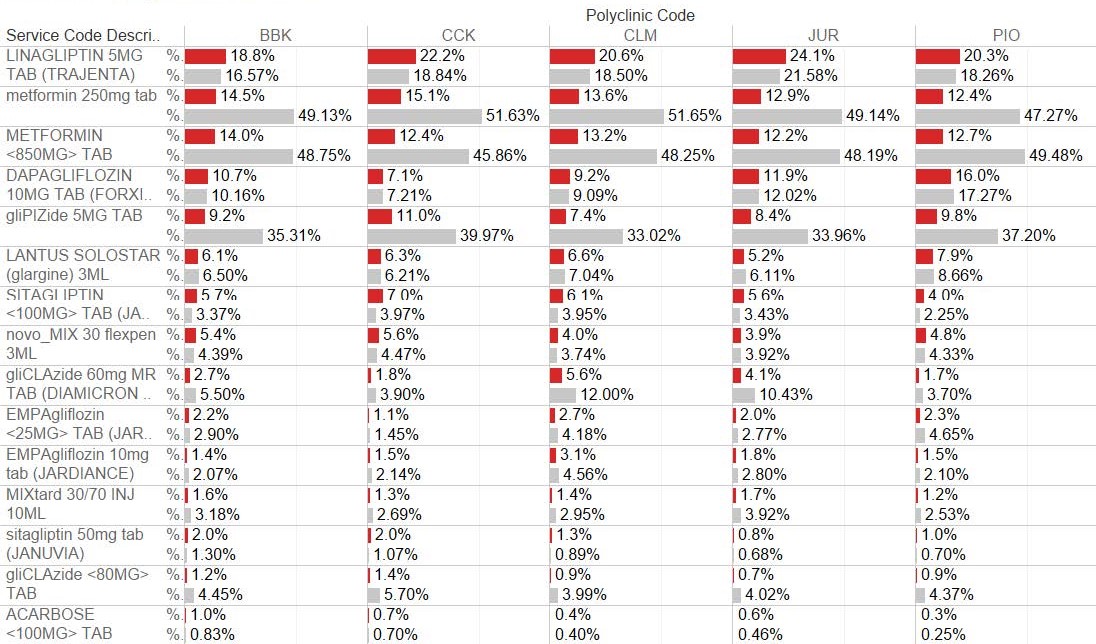
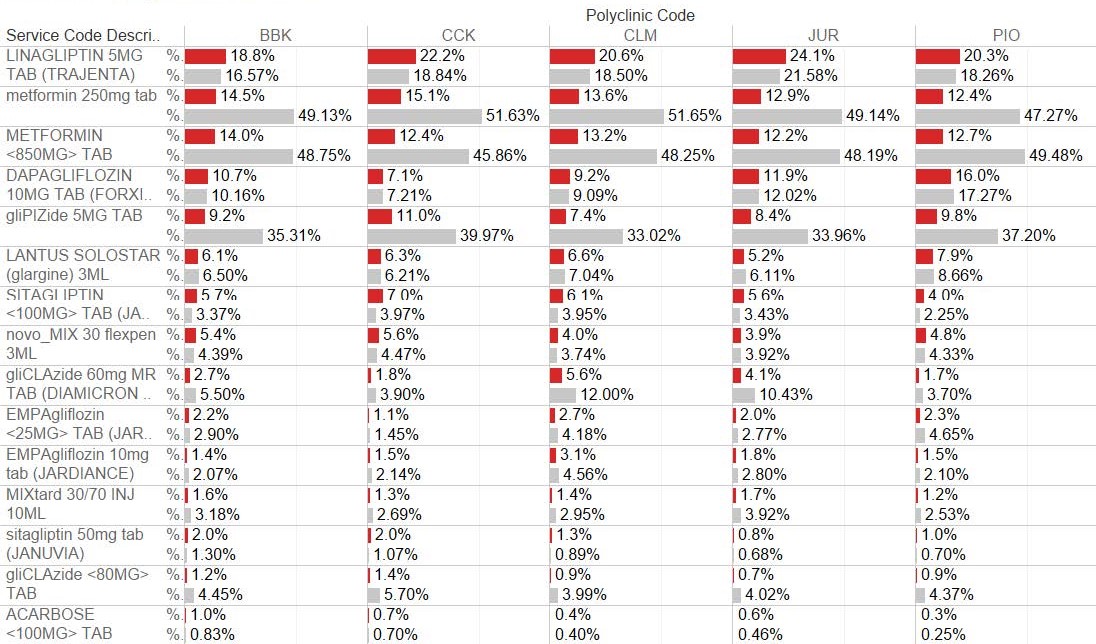
Breakdown of drugs used (2020)
We observed variability in CQI across the clinics, mainly attributed to eye assessment, BMI measurement and HbA1c control. There was a dip in CQI in 2020, mainly from BMI measurement and annual eye and foot assessment. This coincided with the COVID pandemic and some patients postponed their follow-up and eye and foot assessment appointments.
The bill size was comparable across the clinics, and there was an increase in bill size in 2020 attributed to the use of dipeptidyl peptidases 4 inhibitors (DPP4i) such as linagliptin and sitagliptin.
The use of sodium glucose cotransporter 2 inhibitors (SGLT2i) such as dapagliflozin and empagliflozin is lower and is increasing.
Conclusion
The value-driven outcomes dashboard is a useful tool for NUP and clinic leadership to understand outcome and bill size variability.
Our approach to make use of electronic data to generate the dashboard enables the clinicians to focus on identifying and carrying out value improvement initiatives without the hassle of manual data gathering.
With integration with hospital data, we can also study the impact on patient outcomes such as end organ damage, hospital admissions and premature mortality The VDO dashboard will enable us to monitor the use of SGLT2i in future and their effects on cardio-renal complication rates.