Starting on insulin
You might be reading this because your doctor has recommended starting you on insulin treatment. We aim to provide you with essential information about insulin and address any questions you may have about its use.
Why might you need insulin?
You may have been diagnosed with Type 1 Diabetes. In Type 1 diabetes, the body is unable to produce insulin, so insulin needs to be replaced through injections.
If you have Type 2 Diabetes, you may have previously achieved blood sugar targets with diet, exercise, and non-insulin medications. However, over time, your body will produce less insulin. Eventually, many individuals with Type 2 diabetes require insulin therapy to keep their blood sugar levels stable.
For some individuals, insulin therapy may be recommended right from the time of diagnosis based on their unique situation. Sometimes, because the body does not produce enough insulin, oral medications will be ineffective at maintaining blood sugar levels within the target range, making insulin injections necessary.
How does insulin work?
Insulin is a hormone produced by your pancreas that helps regulate blood sugar levels. After you eat, your body turns carbohydrates into glucose, which enters your bloodstream. Insulin acts like a key, allowing sugar to enter cells and be used for energy. This process helps to lower blood sugar levels.
How might insulin improve my life?
Taking insulin can improve your life in several meaningful ways. Many people find that achieving target blood sugar levels helps them feel more energetic and better able to participate in daily activities. If your blood sugar levels are very high, starting insulin can relieve symptoms such as tiredness, persistent thirst, and frequent urination.
Additionally, insulin therapy helps you better manage your blood sugar levels, reducing the risk of serious complications in the future. While it requires some initial adjustment, insulin therapy has the potential to enhance your overall well-being and quality of life.
Which type of insulin is best for me?
There are many types of insulin available in Singapore. They are different in terms of how quickly they start acting (onset of action), and how long their effect lasts (duration of action).
Your healthcare team will work with you to select the right type and combination of insulin that best fits your individual needs and lifestyle. This will take into consideration your health condition, daily routines, eating habits, activity levels, and overall health goals.
Types of insulin available in Singapore -
| Types of insulin | Onset of Insulin Action | How is it administered? | Duration of insulin action |
|---|
| Rapid-acting insulin | 10 - 20 minutes | Taken with a meal | 3 - 5 hours |
| Short-acting insulin | 30 minutes | Taken before a meal | 6 - 8 hours |
| Intermediate-acting insulin | 2 - 3 hours | Taken once to twice a day | 13 - 16 hours |
| Long-acting insulin | 2 - 4 hours | Taken once a day | 24 hours |
| Ultra long-acting insulin | 6 hours | Taken once a day | More than 24 hours |
| Pre-mixed insulin (mixture of rapid/short-acting and intermediate/long-acting insulin) | 10 - 30 minutes | Taken twice a day before meals | 18 to 24 hours or longer |
When you are started on insulin, your healthcare team will provide you with:
- A customised insulin plan
- Specific dosing recommendations and adjustments based on blood sugar levels
- Education and instructions on how to perform insulin injections
Having an insulin regimen personalised to your unique situation can optimise blood sugar control while allowing for flexibility and maintaining quality of life. Your healthcare team will support you throughout the process of starting insulin treatment. They will also help monitor your condition and adjust your insulin dose as needed.
How much insulin will I need?
Each person's insulin needs are unique and personalised. The amount of insulin required and the number of injections per day can vary based on several factors specific to your situation. These include the type of diabetes you have, your daily routines and eating patterns, how long you have been living with diabetes, and whether you also take any oral medications to help manage your blood sugar levels.
Some individuals may need just one injection of long-acting insulin per day, while others might require twice-daily premixed insulin. Additionally, some people may need a combination of long-acting insulin once a day and quick-acting insulin before meals.
Frequently Asked Questions
It is common to have questions when starting insulin treatment. Here are answers to some frequently asked questions:
- Does starting insulin mean that I am not managing my diabetes well?
As Type 2 Diabetes progresses, your body will produce less insulin over time. This decline is a normal part of the disease process and is not a personal failing. Starting insulin does not mean you have mismanaged your diabetes care. In fact, using insulin can help you reach your long-term health by bringing your blood sugar levels into target range.
- How can I minimise pain from insulin injections?
Here are some tips to help make injections less painful:
- Allow insulin to reach room temperature before injecting.
- Use a new needle for each injection and inject at a 90-degree angle.
- Speak to your healthcare team to determine the right needle length for you.
- How do I store my insulin?
- When you bring insulin home from the pharmacy, store all unopened insulin in the fridge (not the freezer).
- When you open a new insulin vial or pen, write the date on it.
- Keep opened vials and pens at room temperature.
- Do not leave the insulin in the car or exposed to direct sunlight.
- Discard the opened vial or pen 28 days after opening.
- For some brands of cloudy insulin, discard the insulin pen when fewer than 12 units remain. Check with your healthcare team if this applies to the brand you are using.
- Can I exercise if I am on insulin treatment?
Exercise has many benefits, including helping you manage your blood sugar levels with fewer medications. However, exercise can also increase the risk of low blood sugar (hypoglycaemia) if you are on insulin treatment. To avoid hypoglycaemia during exercise, you may need to take additional precautions. Consult your healthcare team to learn about these precautions. Additionally, it is advisable to postpone exercise if you have low blood sugar before starting your workout.
- Do I need to monitor blood sugar readings when on insulin?
Monitoring you blood sugar readings when you are on insulin treatment has several benefits. It allows you to:
- Confirm if you are having low blood sugar (hypoglycaemia) or high blood sugar (hyperglycaemia) at any given time.
- Understand how your body responds to food, medications, and other factors like activity levels and stress.
- Make better decisions on a daily basis to keep your blood glucose within an optimal range.
- Enable your healthcare team to adjust your insulin doses to achieve your target blood sugar levels.
- Can I travel with insulin?
Yes, you can and should bring your insulin with you when you travel. Find out how to properly transport insulin and prepare for your trip here.
- Does being on insulin means I am not allowed to drive?
Most people with diabetes who have stable blood sugar levels can drive safely. However, it is important to consult your doctor to ensure you are fit to drive. For more information, refer to the driving safely with diabetes section.
- I am keen to fast for Ramadan, can I still fast while on insulin?
We encourage you to consult your healthcare team at least one month before Ramadan. They can guide you on how to fast safely and determine if any adjustments to your diabetes medications are needed beforehand. For more information, refer to the Diabetes and Ramadan section.
How do I inject insulin?
As you start insulin treatment, your healthcare team will guide you on how to administer insulin using either an insulin pen or a vial and syringe. With practice, you will become more confident and comfortable with the injection process.
Instructions on injecting insulin -
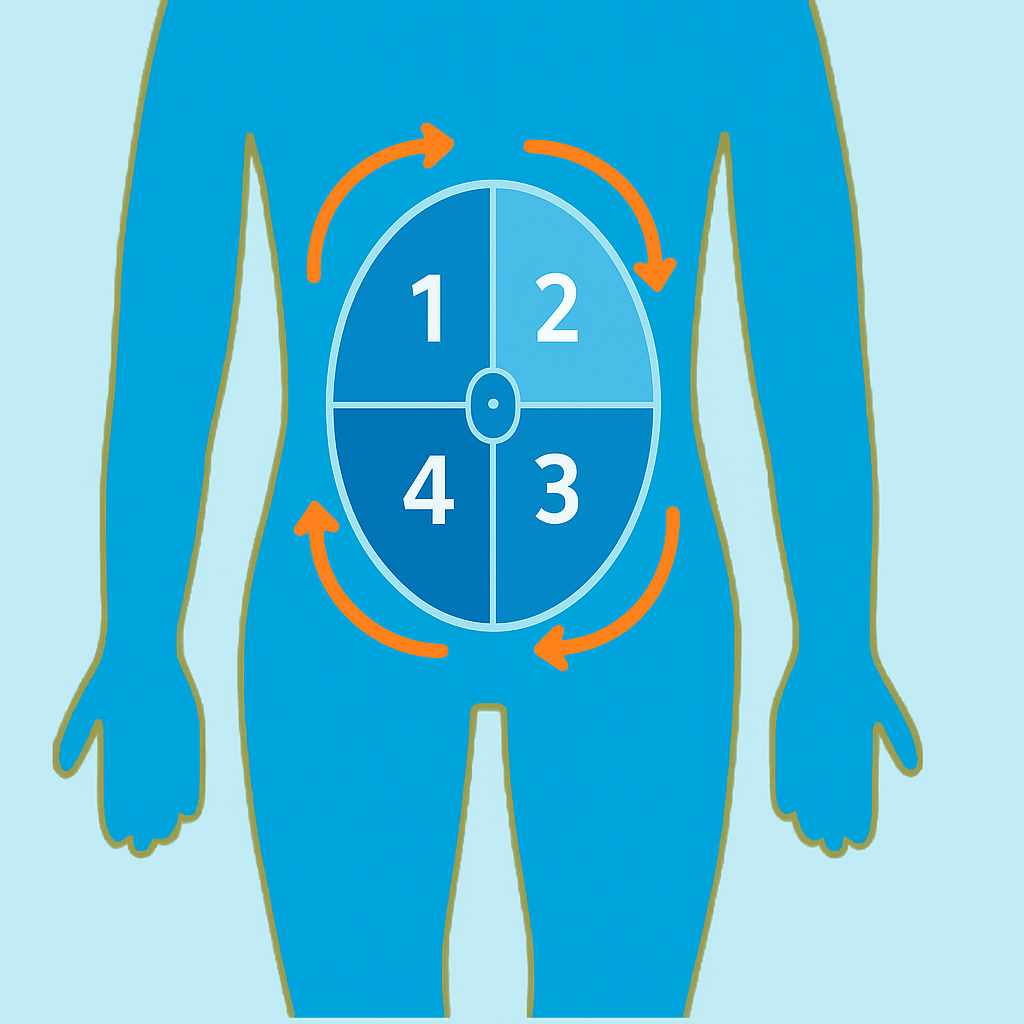
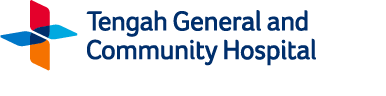
Insulin injection site
Insulin should be injected into subcutaneous (fat) tissue just below the skin, not into muscles. The best site for injecting insulin is the abdomen, as insulin absorption is fastest and most consistent there.
Always use a new needle with each injection to avoid scarring and risk of infection.
Rotation of the injection site
- Rotate the injection site within the same area to avoid developing “fatty lumps” (lipohypertrophy).
- When rotating within one area, space each injection about one finger’s breadth apart.
- Avoid injecting insulin into areas that will be used for exercise, such as the arm or thigh.
- Do not inject insulin into hardened or lumpy areas.
Credit: Image from Diabetes Hub NDRM
Managing the side-effects of insulin treatment
Insulin treatment may cause some side effects. Understanding these potential effects and knowing how to manage them can help you stay on track with your treatment.
Hypoglycaemia (Low blood sugar)
Low blood sugar, or hypoglycaemia, occurs when your glucose levels drop below 4.0 mmol/L. For more information on how to recognise and treat hypoglycaemia, as well as when to seek immediate medical attention, click here.
Low blood sugar can occur while on insulin if you:
- Delay eating or skip a meal
- Take too little “starchy” carbohydrates in the meal
- Drink excessive alcohol or drink on an empty stomach
- Exercise more than usual
- Have poor appetite from being sick due to illness, such as flu, food poisoning, or a urinary tract infection
For tips on how to prevent hypoglycaemia, click here.
If you experience frequent episodes of low blood sugar, it is important to consult your healthcare team quickly. Together, you can reassess your insulin regimen and adjust the dosage or timing of your medications as needed.
Skin changes at injection site
Repeatedly injecting insulin in the same spot can cause lumps to develop under the skin, which can reduce insulin absorption. To avoid this, use a different injection site for each dose. Before injecting, inspect and feel the area to ensure there are no lumps or skin changes. If you find any lumps, choose a different injection site.
Weight gain
Insulin treatment can sometimes lead to weight gain because it may result in consuming more calories than needed, with the excess converted to fat. However, it is possible to maintain a healthy weight while on insulin. Do not skip your insulin doses due to concerns about weight gain, as this can lead to harmful high blood sugar levels.
To manage weight gain while on insulin, consider the following strategies, and discuss them with your healthcare provider:
- Adjust caloric intake: Reduce the number of calories you consume at each meal. If you plan to eat less, your insulin doses may need adjusting.
- Increase physical activity: Exercise can help manage weight. Depending on the type, intensity, and duration of your workouts, you may need to adjust your insulin doses and snacks to prevent low blood sugar.
- Explore additional medications: Your healthcare team might prescribe other diabetes medications alongside insulin that can help prevent weight gain or even promote weight loss.
Proper Disposal of Sharps
How do I safely dispose of sharps (pen needles, syringes & lancets)?
To protect your loved ones and waste collectors from injury, it is essential to dispose of used syringes, insulin pen needles, and lancets (small needles used for blood sugar testing) safely and correctly.
Key tips for safe disposal:
- Do not reuse used needles or lancets.
- Avoid throwing loose used sharps directly into the trash.
- Do not place used needles or lancets in the recycling bin.
- Immediately place all used sharps into a proper disposal container after use.
What kind of container should I use?
- Use a hard plastic or metal container, or purchase a sharps container from the pharmacy.
- Ensure the container is puncture-proof with a tight-fitting lid.
- The container should be able to stand upright and be leak-proof.
- Suitable alternatives include an empty detergent bottle or a sturdy metal tin.
- Clearly label the container with "Used Sharps" to prevent confusion.
When should I dispose the container?
- Seal the container tightly when it is about three-quarters full.
- Use tape to secure the lid if necessary.
- Once the container is full, dispose of it in the trash or down the chute (following local guidelines).
Additional Resources
Back to 'Managing Diabetes' >