It is believed generally that constipation and straining to have bowel movements promote Haemorrhoids and that hard stools can traumatise existing Haemorrhoids. It is recommended, therefore, that individuals with Haemorrhoids soften their stools by increasing their fluid and fiber intake in their diets. This is recommended for all patients who have Haemorrhoidal symptoms and can be the only treatment required for patients with first degree Haemorrhoids.
Vasoconstrictors applied to the perianal area may reduce swelling, pain and itching due to their mild anesthetic effect.
Daflon is a Micronised Purified Flavonoid Fraction (MPFF) that works better than fiber supplements. Its efficacy is deemed to be equivalent to a rubber-band ligation alongside the intake of fiber supplement in stopping anal bleeding due to Haemorrhoids.
Rubber band ligation
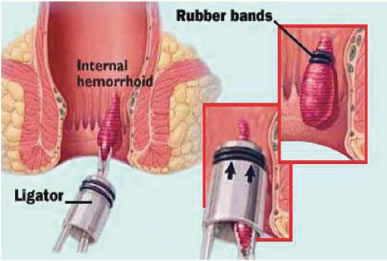
Rubber band ligation
The principle of ligation with rubber bands is to encircle the base of the Haemorrhoidal anal cushion with a tight rubber band. The tissue cut off by the rubber band dies and is replaced by an ulcer that heals with scarring. It can be used with first-, second-, and third-degree Haemorrhoids. Symptoms can recur several years later, but usually can be treated with further ligation.
The most common complication of ligation is pain, but it tends to be mild.
However, if the rubber band is applied too distally, the pain is immediate and severe. Bleeding one or two weeks after ligation occurs occasionally and can be severe. Rarely, cellulitis can begin in the tissues surrounding the anal canal. These rare infectious complications may occur in patients who have defective immune systems from chemotherapy, diabetes, and AIDS.
Diathermy Haemorrhoidectomy
Surgical removal of Haemorrhoids (Haemorrhoidectomy) usually is reserved for patients with third or fourth-degree Haemorrhoids. During Haemorrhoidectomy, the internal and external Haemorrhoids are excised using diathermy. The wounds left by the removal are left open. This is performed as a daycase procedure. Post-surgical pain is the major problem with Haemorrhoidectomy. The addition of NSAIDs enhances the relief of pain. Delayed Haemorrhage 7 to 14 days after surgery occurs in 1-2% of patients. Wound infections are uncommon after Haemorrhoid surgery. Abscess occurs in less than 1% of cases.
However, patients commonly complain of discharge postoperatively and this is expected as the wounds are left open. If the wounds look clean, they do not necessarily need antibiotics. Patients should be advised to keep the area clean and dry, and avoid topical applications of ointments or powder.
Stapled Haemorrhoidectomy
Stapled Haemorrhoidectomy is a technique developed in the early 1990s but is a misnomer since the surgery does not remove the Haemorrhoids but, rather, the abnormally lax and expanded Haemorrhoidal supporting tissue. The arterial blood vessels that travel within the expanded Haemorrhoidal tissue are cut, thereby reducing the blood flow to the Haemorrhoidal vessels and reducing the size of the Haemorrhoids.During the healing of the cut tissues around the staples, scar tissue forms, and this scar tissue anchors the Haemorrhoidal cushions back to their normal position higher in the anal canal, thus effectively performing an anopexy.
External Haemorrhoids are not removed, however. Hence, this procedure is best suited for circumferential third or fourth Haemorrhoids, with minimal external components. It is associated with much less pain than a traditional Haemorrhoidectomy, and patients usually return earlier to work.
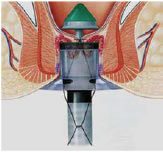 Fig 1
Fig 1
Although rare, there are risks that accompany this procedure:
- If too much muscle tissue is drawn into the device, it can result in damage to the rectal wall.
- The internal muscles of the sphincter may stretch, resulting in short-term or long-term dysfunction.
- As with other surgical treatments for Haemorrhoids, cases of pelvic sepsis have been reported following stapled Haemorrhoidectomy.
- Persistent pain and faecal urgency after stapled Haemorrhoidectomy.