Background
Most children who have end-stage renal failure in Myanmar either have no access to dialysis or have to stay in hospital for years for chronic hemodialysis (since their home villages are too far away for regular commute) until they reach adult age when they can be transferred to the adult dialysis centres or be eligible for renal transplantation in the adult unit. Before 2017, renal transplantation was not an option for children in Myanmar due to lack of expertise. For long-term sustainability, and for better quality of life, renal transplantation should be made available to children in Myanmar. The Mentoring Centre (MC) team therefore took on the task of transferring their expertise to the Emerging Centres (EC) teams. Aim
Our aim was to set up a new sustainable renal transplant programme in the two ECs, which are currently the main tertiary referral centres in the country. We wanted sustainability, which means we wanted to establish expertise of the multidisciplinary team with good workflow and adequate facilities so that the EC teams can ultimately perform the transplants independently.
The Yangon
Emerging Centres (EC) and Mentoring Centre (MC) team
Achievements
Work Processes and Materials (for sustainability)
We ensured the EC teams have the protocols and processes for the transplant. These included:
· Pre-transplant work-up of the donor and recipient
· Ethics and consent forms
· Perioperative management
· Post-operative monitoring and immunosuppression
· Hand-written charts for ICU nurse hourly monitoring of vital signs and fluid balance, and post-transplant clinic follow-up monitoring chart were created with the help of MC.
Steps to ensure good graft survival
We also made great efforts to ensure good long-term graft survival by the following steps:
1) Continuity of funds for medications and follow-up visits and investigations. There are charity funds designated to fund the medical bills for each recipient
2) Adequate education of the patient and families is required to ensure they are thoroughly counselled and educated. The EC doctors also wrote patient education booklets to educate patients and families of potential and current transplant problems. The whole syllabus on transplant education, and even transplant consent form, was modelled from the materials from MC team.
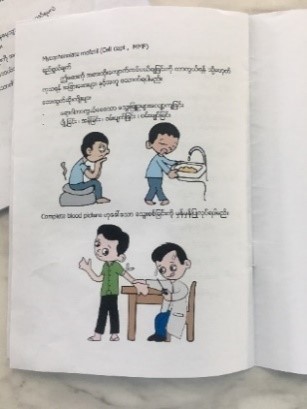
3) Home visits by EC team in the rural hometowns of the recipients are done to ensure their living conditions are of adequate standards to prevent infections. The team ensures food, water and sanitary standards were present in the homes. If conditions were not satisfactory, they will advise on improvement. For the first transplant performed in Mandalay, the EC doctors rallied the villagers to raise funds to build a proper toilet for the patient.
4) Contact with the local village primary physician remained essential as the EC team maintained very close contact with the primary healthcare providers in the district hospitals to ensure they are aware of the patients’ conditions and to advise them on the first steps to be done should the patients present to them with acute illnesses like gastroenteritis. Emphasis was made on adequate hydration and antibiotic coverage if there is suspicion of acute bacterial infections prior to sending the patients to the ECs for further management.
Close Communication between ECs and MC
We have maintained extremely close links between EC and MCs. At any time, there were at least one or two training fellows from EC undergoing training in MC, sponsored by International Paediatric Nephrology Association (IPNA). These fellows served as very important links as they could convey the requirements and instructions from MC team to the EC teams.
Communication was conducted via the following modes:
- Weekly Friday morning and ad-hoc GoToMeeting web meetings between ECs and MC
- WhatsApp group chats among EC and MC doctors; WhatsApp calls
- Emails
- Visits by multidisciplinary team from MC to ECs
New initiatives / Benefits in ECs as a result of the transplants or ISN SRC collaboration 1) Recognition and support from Ministry of Health and Sports, Myanmar- The Minister of Health and Sports, Myanmar (MOHS) visited the hospital on the day of the first transplant, which opened up communication channels with the MOHS, increasing their awareness on kidney disease in children.
- The visit facilitated funding from MOHS for the transplants including equipment and instruments.
- After the transplant in Yangon in Jan 2018, there was a meeting set up the following week between Prof. Yap Hui Kim (from MC), Prof. Aye Maung Han (from Myanmar MOHS), Prof. Yi Yi Khin and Associate Prof. Cho Cho San (from EC). MOHS approved the proposal for “Prevention of chronic kidney disease, management of acute kidney injury and quality development in prevention and treatment of pediatric renal diseases” that was put forward.
- A separate meeting was set up in August 2018 with MOHS to discuss future transplant costs and instrument support. Support (including financial) had been granted for future transplants, and for workshops to teach rural / suburban physicians how to perform acute peritoneal dialysis in children (in collaboration with MC doctors).
2) The “Yangon Children Hospital Kidney Foundation” was set up by EC paediatric nephrologists to support chronic kidney disease and renal transplantation.
3) Increased general awareness of kidney disease in children through news articles in major Myanmar newspapers reporting on the paediatric renal transplant in Yangon.